|
The
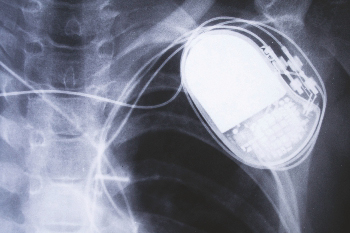
Biocompatibility and Biostability of the Materials
Chosen for Your Device will Affect its Clinical Success.
(Curtsey : Lubrizol)
A material’s biocompatibility and
biostability profile is a critical consideration in the
development of your next medical device. The specific
requirements of the medical device greatly influence the
choice of appropriate material, as biocompatibility and
biostability performance always need to be considered in the
context of the end-use application.
To help ensure positive patient
outcomes and mitigate potential risks when designing your
device, your team should consider numerous factors that
influence device biocompatibility and biostability during the
material selection phase of development. In this overview, we
will highlight the most important factors to help guide you to
success in choosing the right polymer for your device.
THE MOST COMMON FACTORS
AFFECTING BIOCOMPATIBILITY AND BIOSTABILITY -
The biocompatibility and
biostability requirements of a particular medical device are
dependent upon its application-specific design and performance
requirements. For example, the material utilized in a
long-term cardiac implant has a stringent set of
biocompatibility and biostability requirements designed and
tested around extended blood and/ or tissue contact.
Conversely, a temporary surgical application may not consider
biostability as a critical factor due to the limited duration
of use. Below are key application-specific biocompatibility
and biostability factors to consider.
Factor 1: DEVICE LOCATION
The location of use within the
body determines the chemical environment that the material
sees, which in turn influences the material performance
requirements. For example, in direct blood contact, the body’s
immune response (via the white blood cells), can create a
harsh oxidative environment at the material surface as the
white blood cells try to phagocytize (consume) the foreign
material. Therefore, devices in long-term direct blood contact
generally need materials with excellent oxidative resistance.
Conversely, devices in contact with skin may not experience
the same level of oxidative pressure as in blood contact, so
materials with resistance to hydrolysis (degradation by water)
may be appropriate for construction. Furthermore, medical
devices in contact with extreme pH environments, such as in
the gastric system, require materials that can perform under
chemically harsh environments.
Factor 2: DURATION OF DEVICE
CONTACT
A device’s duration of use
determines biostability requirements and can dictate
biocompatibility evaluation endpoints. For example, a
short-term catheter that may only be in the body for several
hours will not be subject to the same evaluation endpoints as
an orthopedic implant designed to perform for years. From a
biostability perspective, the chemical resistance required in
an environment (as described above – oxidative, hydrolytic,
extreme pH, etc.) is dependent on exposure time. Therefore, a
device which needs to remain stable for hours may require
different materials than a device used in the same environment
that needs to remain stable for years. From a biocompatibility
perspective, devices that are in contact with the body for an
extended period will require different biocompatibility
assessments including chronic toxicity, and genotoxicity.
Additionally, potential degradation byproducts and
extractables from the device materials may also need to be
evaluated either via chemical or biological assessment.
Factor 3: MECHANICAL ACTIVITY
AND REQUIREMENTS
The mechanical load to which a
device component will be subjected during use (tension versus
compression or static versus dynamic) can have significant
implications on its biostability. Some polymers under constant
or repetitive strain break down more quickly from biological
conditions than unstrained polymers. For example, the
mechanical requirements of an orthopedic implant are
significantly different than material used in temporary
drainage tubes. In this situation, additional polymer-specific
considerations may need to be specified to ensure proper
performance.
Factor 4: DEVICE CONTACT WITH
DELICATE TISSUE
If the device is contacting
delicate tissue, the mechanical action of the device against
tissue can cause a physical biological response (i.e.
swelling, tearing) that can impact the overall
biocompatibility of the device. In this case, the mechanical
properties of the material are as important as the chemical
compatibility and should be considered during the initial
phases of material selection for a device.
Factor 5: LOCAL EFFECTS AT THE
BIOMATERIAL INTERFACE
Depending on a medical device’s
application, a determination needs to be made as to whether
protein adsorption, fouling, and bacterial adhesion are a
concern. These factors can significantly impact device
performance, and material selection can be tailored based on
the requirements at the biomaterial interface.
Factor 6: DEVICE STERILIZATION
Certain sterilization methods can
change chemical and physical properties of device materials,
potentially impacting their performance, including
biocompatibility and biostability. Some thermoplastic polymers
are negatively impacted by the heat, pressure, and humidity of
autoclave (steam) sterilization methods. In extreme cases,
autoclave sterilization can generate unwanted degradation
byproducts in some polyurethanes. Other methods such as gamma
or e-beam radiation are typically appropriate for
thermoplastic polymers, but selecting an appropriate radiation
dosage can be important to prevent chemical changes to the
device materials.
Factor 7: OVERALL DESIGN AND
MANUFACTURING PROCESSES
Lastly, your team should
holistically consider the design and manufacturing process of
the device. What are the implications of other materials (i.e.
conductive metals) contained in or in contact with the device?
Will any additional chemical additives be required (i.e.
plasticizers)? Will any coatings or textures be applied to the
final version of the device? Will components be thick or thin
walled? What processes will be utilized to manufacture the
components? These design decisions can greatly impact
biocompatibility and biostability of the final product, which
is why it is important to partner with a trusted materials
expert that can help guide you through these questions.
PARTNERS FOR BETTER POLYMER
PERFORMANCE
Lubrizol is equipped with decades
of knowledge and experience to provide OEMs with the insight
to understand how device design and end use will determine
component biocompatibility and biostability requirements and
how this must drive material selection to create a clinically
safe and effective device. For more information contact
Rajnish.Singh@Lubrizol.com;
Mittal.Shah@Lubrizol.com.
|
